On April 22, 2003, my son Adam was diagnosed with testicular cancer. Adam was only 18 years old and looking forward to his future after finishing high school.
Adam spent the rest of the school year in a chemotherapy centre. In the months that followed, Adam told me a story of when he was in grade 10 and his testicle swelled; at the time, he was too embarrassed to say anything about it. Throughout the long hours of chemotherapy, Adam dreamt of educating other young men about testicular cancer — going into schools and teaching young men not to be afraid of telling someone if they suspected they had a problem in their testicles.
On November 9, 2003, just 7 months after his diagnosis, Adam died. After he passed away, I vowed to make my son’s dream come true and, with the help of friends and family, I formed [highlight]Testicular Cancer Canada[/highlight].
We’re committed to raising awareness about testicular cancer while supporting those affected by the disease. We equip men with the tools they need to identify testicular cancer early so they can avoid painful, lengthy treatment and life-altering complications like impotence and infertility.
To contribute to our cause, visit our Donate section. With your help, we can continue our mission to educate and support. Thanks for reading.
[divider]
Diagnosing testicular cancer
Diagnosis is the process of finding the underlying cause of a health problem. If cancer is suspected, the healthcare team will confirm if it is present or not, and what type of cancer it is. The process of diagnosis may seem long and frustrating, but it is important for the doctor to rule out other possible reasons for a health problem before making a cancer diagnosis.
Diagnostic tests for testicular cancer are usually done when:
- the symptoms of testicular cancer are present
- the doctor suspects testicular cancer after talking with the man about his health and completing a physical examination
Many of the same tests used to initially diagnose cancer are also used to determine the stage (how far the cancer has progressed). Your doctor may also order other tests to check your general health and to help plan your treatment. Tests may include the following:
Medical history and physical examination
The medical history is a record of present symptoms, risk factors and all the medical events and problems a person has had in the past. The medical history of a person’s family may also help the doctor diagnose testicular cancer.
In taking a medical history, the doctor may ask questions about:
- a personal history of
- previous testicular cancer
- abnormal development of the testicles
- cryptorchidism – undescended testicle
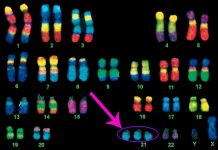
- Klinefelter syndrome – a genetic condition that causes the testicles to waste away (atrophy) and not make sperm, a man’s breasts to grow and a lack of male sexual characteristics
- occupational or environmental chemical exposure
- past medical or surgical treatment for a testicular disorder
- history of any injury or trauma to the testicles
- decreased fertility
- a family history of testicular cancer
A physical examination allows the doctor to look for any signs of testicular cancer. During a physical examination, the doctor may:
- evaluate the man’s general health
- examine the testicles and scrotum for lumps, swelling or pain
- check for enlarged lymph nodes in the groin, neck and armpit
- listen to the lungs
- feel the abdomen for an enlarged liver or other lumps